"Discover our virtues that we believe set us apart."
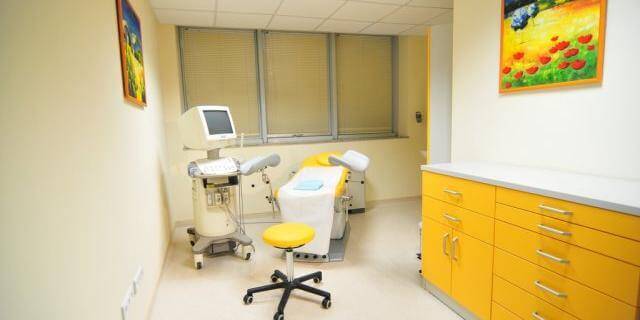
Turkey has become a popular destination for anyone aspiring to have a child of their own through in vitro fertilization (IVF) and treatment. It is a draw with its successful clinics and affordable prices. Through their years of experience, Brüksel IVF and Women's Health Center, in the person of their erudite specialists, have communicated the wonderful news of conception to over 30,000 families worldwide.
After many years as Head of the Endoscopic Surgery and IVF Department at the Brussels Edith Cavell Medical Institute and Hospital Français in Belgium, and after the extensive experience he gained there, Prof. Dr. Yüdel Karaman founded the Brüksel IVF and Women's Health Center in Istanbul, Turkey in 2007.
Brüksel IVF and Women's Health Center has world-class medical equipment and a team of specialists in the field of women's health and IVF. After more than 30 years of European experience and as the founder and medical director, Prof. Dr. Karaman precisely selects the staff working at the center.
Why choose Brüksel IVF and Women's Health Center?
- Personal approach to each patient - The hospital unconditionally believes in the claim that every man or woman who undergoes treatment for infertility is a unique case. Every couple that comes to the center to get help has a unique medical history and their own problem and reason for infertility. It is our understanding that a personalized treatment plan for each case is the foundation of success.
- World-class embryology laboratory - Embryologists and technicians who work on eggs, sperm and embryos are critical to assisted reproductive processing. They must be as experienced as the clinical experts who supervise the treatment. Scientists working in the embryology laboratory are expected to have the highest level of expertise in the field. In addition to excellent laboratory personnel comes the quality of equipment, high level of technology and state of ventilation, which are important criteria for any successful world-class laboratory. The hospital not only follows innovations in the field of assisted reproductive treatments, but innovates in the field by relying on the tried and tested personalized treatment philosophy.
- Embryo Recording Support System
- Centre for Advanced Endoscopic Surgery
- Brüksel IVF and Women's Health Center has well-trained experts in assisted reproductive treatment. The founder, Prof. Dr. Eugel Karaman, was involved in the first in vitro fertilizations in Brussels and is one of the pioneers of many developments in this field since 2008. After more than 30 years of European experience, Prof. Dr. Karaman staffed the centre with particular care.


Several important steps are followed for successful treatment:
- Free initial online consultation with a specialist. During this first contact with the patient, the medical history and current results of all tests are reviewed to see what the patients' real expectations are. This consultation is a good opportunity for any questions the patient may have about the process to find their proper answer.
- The first visit to the clinic for medical consultation follows.
- Screening tests are the next step - During the online medical consultation, the full list of tests required for treatment will be provided. If it is not possible to perform these tests locally, they can be performed during the patient's visit to Brüksel IVF and Women's Health Center.
- Spermogram - men are required to give a semen sample at the clinic to obtain an accurate result.
- Preparation of a personalized treatment plan and treatment follow-up - After the first visit, a personalized treatment plan will be provided. The length of treatment may vary depending on the type of treatment the patient will undergo. A treatment plan is always developed to fit the patient's schedule.
- Second visit to the clinic - undergoes either the insemination procedure, egg puncture or embryo transfer, depending on the treatment.
- Pregnancy test - After the procedure, the patient is given detailed information on how to care for herself after treatment and instructions on how to continue with her medication and when to perform the pregnancy test (quantitative β-hCG). The medical team liaised with the patient through the pregnancy monitoring with the help of the GP.
The following methods, techniques and tests are applied at the Brüksel IVF and Women's Health Center:
- Freezing of embryos - embryo freezing (vitrification) is usually performed on the 3rd and 5th day. At the discretion of embryologists.
- ICSI - Microinjection - The microinjection method is used in men who have previously had very low or zero chances of fertilizing the egg with conventional IVF treatment. Unlike conventional IVF, where the process is performed with 100,000 sperm and relies on spontaneous penetration of the egg, in Micro-Injection or ICSI, a single sperm cell can be preselected to be injected into the egg. The ICSI procedure is performed with a device called a micromanipulator.
- IMSI - This technique allows the microinjection of sperm without damaging the living sperm cell. IMSI - Sperm Microinjection was first applied at Brüksel IVF and Women's Health Center. Special microscopes are used for this method. In the process using IMSI, the intracellular structures and morphology of the cell nucleus are examined in detail using 6000-8000 times magnification. Thus, the chances of successful fertilization are increased from 25% to 40%.
- Assisted hatching - In vitro fertilization, the thinning or perforation of the outer membrane around the embryo before embryo transfer, is called Assisted Hatching. The purpose of the procedure is to increase the likelihood of implantation. This procedure, especially on the outer membranes of frozen embryos, is essential before treatment. Assisted hatching is performed using a laser. It is a reliable and useful technique.
- Co-culture - Co-culture is a type of auxiliary medium prepared for embryos with intrauterine cells of the woman. A small tissue sample is taken from the uterus on the 21st day of menstruation. The cells contained in this sample are necessary for the attachment and development of embryos. Co-culture provides a rich nutrient environment for embryo development while minimizing harm from toxic waste. It is also believed that a positive chemical interaction occurs between these cells taken from the mother's womb and the embryo. This interaction increases the chances of retaining embryos in the uterus and creating a pregnancy.
- Pre-implantation genetic test (PGS) - Embryos that develop in both normal and in vitro fertilization can contain numerical or structural chromosomal abnormalities, and these abnormalities can often lead to early miscarriages or to compatible or incompatible health problems in the developing baby. Detection of numerical abnormalities (aneuploidies) and structural abnormalities (translocations, deletions and inversions) in embryos is now possible with preimplantation genetic screening (PGS) methods. Briefly, the PGS method allows embryos to be examined prior to transfer to the uterus for chromosomal aneuploidy and translocations. Our center uses the New Generation Screening (NGS) method, which is the most advanced genetic screening test for PGS.
- Intrauterine stimulation - Intrauterine stimulation represents intrauterine scratching. The scratching process is completed in about 1 minute and there is very light bleeding and staining after the procedure. The goal here is to increase the chances of embryo retention by stimulating the inner uterine wall by increasing the release of growth hormones. This method is usually recommended to patients who are unable to conceive after 2-3 high quality embryo transfers.
- Mioxsys system - This is an innovative method of assessing male infertility. The Mioxsys system is the most innovative system that measures the level of oxidative stress that cannot be determined in a spermogram. If the result exceeds the specified limits, the most important thing is to reduce the level of oxidative stress to which the semen is exposed. To this end, the man should improve his quality of life and benefit from supportive antioxidant products to reduce oxidative sterility for at least 3 months.
- MitoScore - MitoScore is one way couples can choose the best of embryos to ensure a healthy baby.
- Micro Tese - (Microdissection - extraction of sperm from the testicles) - This is the most reliable biopsy method. It is usually used in men diagnosed with azoospermia. TESA is a method of obtaining sperm from testicular tissue through a needle.
- Spermchip (sperm microchip) - An innovative approach to sperm selection for IVF.
- Transfer of blastocysts - Embryos that develop in the lab for 5 days are called blastocysts. Blastocyst embryos are produced on the 5th or 6th day after in vitro fertilization. Embryo transfer on day 5 or 6 is called blastocyst transfer.
- PGD - genetic diagnosis - Pre-implantation genetic diagnosis (PGD) is a method used to diagnose the embryo - and whether it is normal in terms of the chromosomes and genetic diseases tested. Embryo biopsy is an important method to test whether the embryo carries any genetic disease or is chromosomally normal. The cell (blastomere) taken from the embryo by biopsy is passed into the genetic part. As a result of the genetic screening, the transfer of normal embryos takes place.
- Globozoospermia - Globozoospermia is the name given to the absence of an acrosome structure in the sperm head region (type I globozoospermia) or a very small acrosome structure (type II globozoospermia).
- One of the most unique methods used is Rosi - The innovative ROSI technique is used in the treatment of azoospermia, a disease causing infertility in men. Men diagnosed with azoospermia, without mature sperm in the semen, can benefit from the ROSI technique. In some patients, mature sperm can be obtained by the TESE technique. The ROSI technique can be used in those patients in whom mature sperm cannot be obtained by TESE. This is the reason it is used in people who have little or no chance of getting results from IVF or other assisted reproductive treatments. Pregnancy success with the ROSI technique is known to be around 20%. It can be said that this is the only option available for people who are diagnosed with azoospermia, and still want to have children with their own cells.
- Hysteroscopy - used in the diagnosis and treatment of intrauterine problems (fibroids, polyps and adhesions). A hysteroscope is a long, thin, lighted device inserted through the vagina into the uterus. It projects an image on a screen and allows the doctor to see and treat the uterus. Intrauterine disorders have a negative impact on embryo implantation. Therefore, eliminating these problems is important to increase the chance of success in IVF treatment.